Never Kill the Wolves: Yellowstone & You
Ecological Complexity, Wolves & H. Pylori, Butterfly Effects, the Microbiome, The Law of Unintended Consequences & Fractal Biology
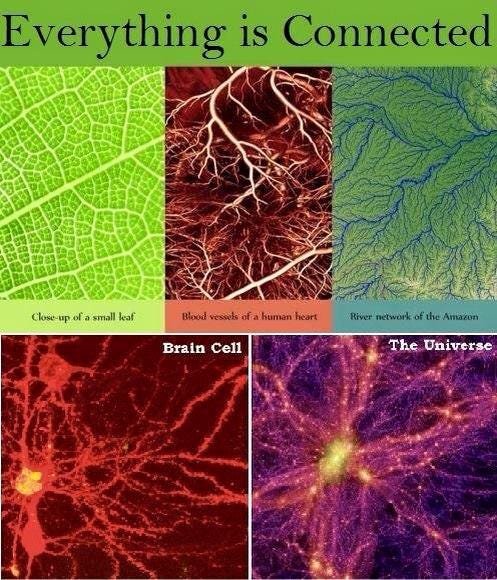
One of the best ways to understand the way our body works is to compare it to a larger ecosystem, e.g. a rainforest or national park.
The ancient Chinese likened the various arteries and veins to bodies of water: wells, streams, rivers. Their analogies illustrate the actual fluid dynamics of blood flow in various blood vessels better than our modern anatomical textbooks.
But the analogies between the body and the macroscopic environment may run far deeper than they knew.
We now know that our human cells are vastly outnumbered by synergistic organisms that live in and on us including bacteria, viruses, parasites, fungi, and archaea. There at least 10s of thousands of different viruses, many thousands of bacteria, hundreds of fungi, 10s of archaea and varying numbers of parasites.
This situation resembles any natural ecosystem comprised of hundreds of animals, thousands of plants, and 10s of thousands of insects.
We know far more about external ecosystems that we have been studying since the dawn of time than we do about the one inside us, which we’ve been closely studying for just the past couple decades, yet we still often make foolish mistakes even in the former.
REROUTING RIVERS
In the mid-20th century, the Soviet government prioritized the production of cotton, often referred to as "white gold," as a key export commodity. Central Asia, particularly Uzbekistan, became the center of this cotton production drive. Cotton is an extremely water-intensive crop, requiring large quantities of irrigation to thrive in the hot, dry climate of Central Asia, so this plan led to significant water shortages in the region.
In the 1960s Alexei Kosygin, the technocratic Soviet Premier hatched a hare brained scheme to reroute Siberian rivers to the area. From the outset the plan faced numerous outsized technical challenges. The project required massive infrastructure, including canals, dams, and pumping stations, to transport water over thousands of kilometers, which posed significant engineering and energy demands. Geological and climatic challenges, such as permafrost, extreme weather, and seasonal flow variability, further complicated construction and operation. The project's enormous cost, technological limitations, and political and social resistance within the Soviet Union contributed to its ultimate failure.
Rerouting rivers at scale is no easy task, yet what a geopolitical superpower failed to do was inadvertently accomplished in the American midwest with one seemingly inconsequential change to the ecosystem in the early 20th century which had cascading butterfly effects that ended up rerouting rivers throughout Yellowstone National Park.
In the late 19th and early 20th centuries, as settlers expanded into the American West, including Yellowstone, livestock ranching became widespread. Native wolves came to pose a significant threat to livestock, particularly cattle and sheep. To protect their livelihoods, ranchers and the government considered wolves pests that needed to be eradicated. As a result, federal and state governments implemented bounty programs, paying individuals to hunt, trap, and poison wolves. Additionally, government agencies like the U.S. Biological Survey conducted organized extermination campaigns. By the mid-1920s, these efforts had successfully eradicated wolves from Yellowstone and most of the contiguous United States.
When wolves were removed from Yellowstone National Park, it triggered a series of dramatic ecological changes.
Since wolves were the apex predator, their elimination first positively affected their primary sources of food: elk, deer and other herbivore whose populations exploded.
The increased herbivore numbers led to overgrazing, particularly of 3 key tree species: willows, aspen and cottonwood.
The roots of these trees played a crucial role in stabilizing riverbanks by anchoring the soil, which helps prevent erosion. They also absorbed excess nitrates and phosphates from the water, reducing the risk of algal blooms that can deplete oxygen levels in the water. The leaves of the trees also provided shade, keeping the water cooler, which also improved the amount of dissolved oxygen, which is of course vital for aquatic life.
The root systems not only gripped the soil, making it resistant to being washed away, but also worked with fallen leaves and stems to trap sediment and organic matter. This created friction that slowed down the flow of water. Moreover, the trees supplied material for beavers to build dams, which further slowed water flow.
Slow-moving water is important because it allows sediments, and other particulates, including heavy metals, to settle out, resulting in cleaner water. It also gives the riverbed more time to absorb water and create a reservoir of groundwater, which is crucial during dry spells, since it can be released back into the river to maintain baseline flow rates. The absorptive capacity of the riverbed also depends on the increased soil porosity from the channels created by the trees widespread root systems.
Without all of these these protective effects, erosion of riverbanks can actually alter the courses of rivers, while making them wider and shallower, which also decreases water quality and harms aquatic species.
Thank you for reading Dr. Syed Haider. This post is public so feel free to share it.
The loss of vegetation also impacted many other species, including birds that needed trees for nesting and insects that consumed the leaves.
Additionally, coyote populations increased in the absence of wolves, because of decreased predation from wolves. This led to a significant decline in pronghorn antelopes, whose fawns were a primary source of food for the coyotes.
The combination of overgrazing, vegetation loss, and altered water systems led to a tremendous loss of biodiversity, with many plant and animal species declining or disappearing.
The removal of wolves disrupted the balance of the ecosystem, making it less resilient to stressors like normal climactic variations (eg dry spells) and human activities such as pollution.
The reintroduction of wolves in 1995 began to reverse these effects, with elk numbers decreasing, willow, aspen, and cottonwood trees recovering, beaver populations rebounding, and overall ecosystem health improving.
In the planet’s ecosystems we have a pretty good idea of which species are native and which are external invaders, but in our bodies we often get confused between the two.
H PYLORI: FRIEND OR FOE vs NATIVE OR NOT?
In the 1970s and early 1980s, Australian physicians Barry Marshall and Robin Warren observed that many patients with gastritis and peptic ulcers had H. pylori bacteria in their stomach lining. At the time, the prevailing belief was that ulcers were caused by stress, spicy food, and excess stomach acid, and the idea that bacteria could survive in the normally highly acidic environment of the stomach was widely dismissed.
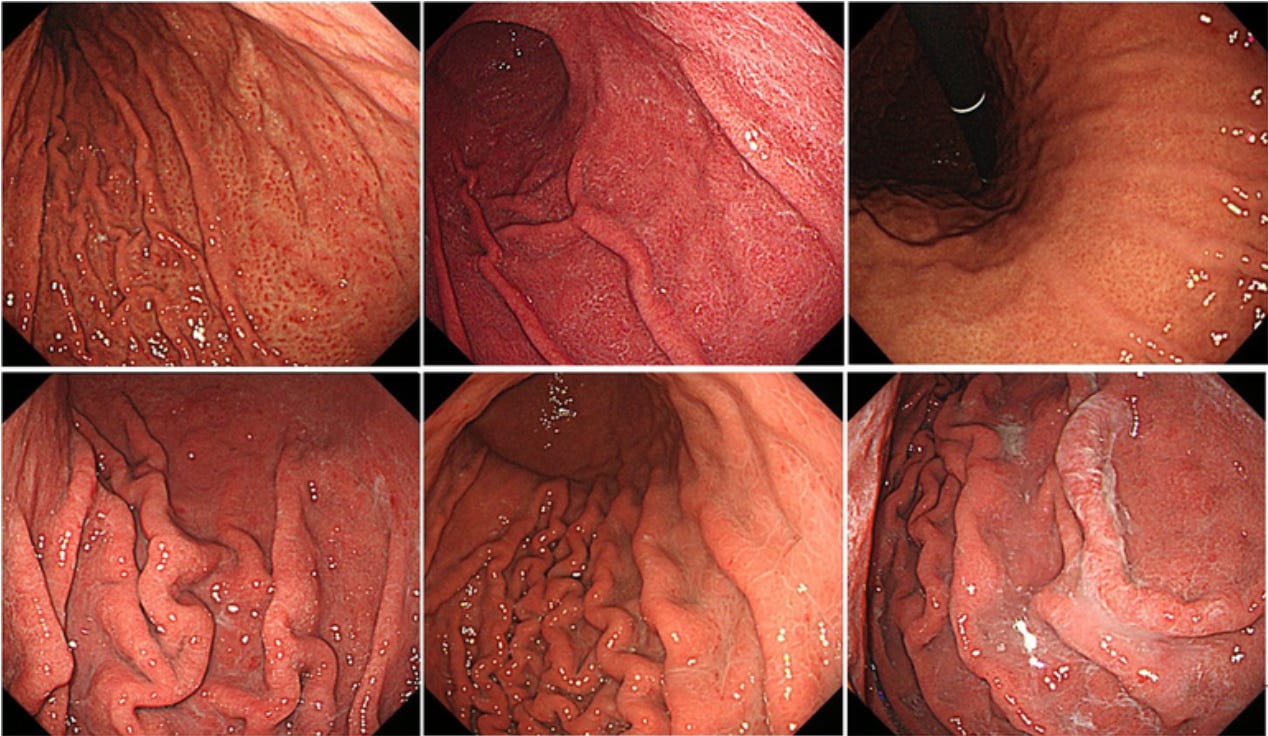
To prove the connection between H. pylori and ulcers, Dr. Marshall conducted a bold experiment on himself in 1984. He drank a broth containing H. pylori bacteria, and within days, he developed symptoms of gastritis, including nausea and vomiting. A subsequent endoscopy confirmed that his stomach lining was inflamed, and H. pylori was present. Marshall subsequently treated himself with antibiotics, which eradicated the infection and resolved his symptoms.
This dramatic self-experimentation was heralded as providing strong evidence that H. pylori could cause gastritis, which could then lead to ulcers.
However, the duration of his symptoms was relatively short, and some critics have suggested that his condition might have resolved on its own without the need for antibiotics. There was no placebo group and no blinding, and of course the sample size was limited to one person—Marshall himself, who expected to get sick, which could have created a self-fulfilling prophecy, or nocebo effect (and what else was in the bacteria “broth” anyway?).
Despite these criticisms, subsequent research has been interpreted as overwhelmingly supported the link between H. pylori and peptic ulcer disease. Numerous controlled studies have purportedely confirmed that H. pylori infection is a major cause of ulcers and that treating the infection with antibiotics can lead to ulcer resolution.
So everything was wrapped up with a neat little bow and put on the shelf complete with all-expenses paid vacation-style medical conferences to Tahiti, autobiographical books, untold numbers of textbook chapters, and numerous prestigious awards culminated by the 2005 Nobel Prize in Medicine.
Yet despite all the fanfare, there were soon rumblings of doubt, though swept under the rug. In the early 90s Dr Julie Parsonnet research had already suggested that in some contexts, H. pylori might have beneficial rather than pathological effects, such as the not so unimportant reduction in the risk of esophageal adenocarcinoma.
Uh oh. Was this an out of the frying pan and into the fire type of situation?
In the late aughts Dr Martin J. Blaser a prominent microbiologist and author of Missing Microbes, found that not only could H. pylori protect against some esophageal diseases including but not limited to cancers, to was also protective against asthma and allergies.
What was going on? Was this a pathogen or a benefactor, or some weird combination of both depending on it’s mood and preference for one human over another?
H. pylori had been in the human stomach for thousands of years before Dr Barry Marshall saw fit to add and immediately subtract it from his own. Despite this long prevalence peptic ulcer disease is not prevalent in preindustrial societies eating their traditional diets, so it’s likely to be, at least in part, a lifestyle disease. But why then does eradicating H. pylori help mitigate ulcers?
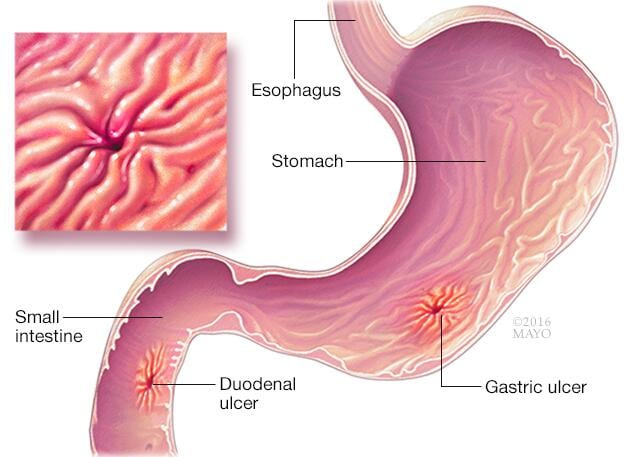
H. pylori can help the stomach maintain its acidity by stimulating the production of gastrin. This is particularly common in colonizations affecting the antrum, the lower part of the stomach. However in colonizations affecting the corpus, or upper part of the stomach, the opposite occurs and acid production goes down. It’s possible that either one or the other was beneficial for particular populations eating particular foods. Many people in modern societies tend to have abnormally decreased stomach acid levels as they age, which could be in part due to loss of H. pylori and might be improved by adding it back in a la Dr Marshall and his H. pylori juice.
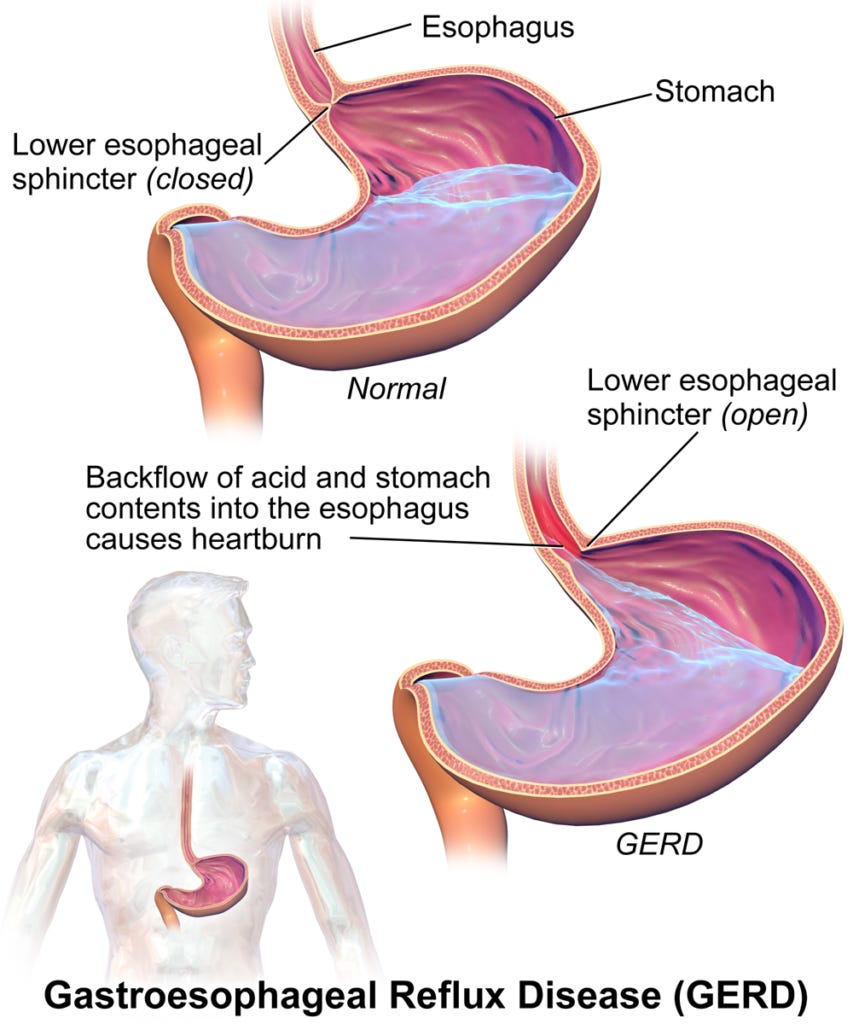
Stomach acid is important not only for digesting food, but for signaling the gastroesophageal sphincter - a functional one way valve between the throat and the stomach - to remain tightly closed and not allow acid to reflux back, which in chronic cases can lead to damage that predisposes to esophageal cancer (this simple physiological fact invalidates the usual treatment of reflux, which is to perpetually decrease and even eliminate stomach acid with over the counter and prescription drugs. In fact the functional treatment of acid reflux is often to increase stomach acid with betaine hydrochloride).
Thank you for reading Dr. Syed Haider. This post is public so feel free to share it.
While the stomach is supposed to be a highly acidic environment in order to break down food and extract nutrients, if the protective mucus coating of the stomach breaks down that acid can lead to an ulcer forming in the exposed stomach lining. So, let’s explain why that might happen.
First of all traditional diets do not contain highly inflammatory components like industrial seed oils, highly processed carbs and proteins, pesticides, and other unnatural chemical constituents that may upset gastric balance to thin the mucus layer and damage the gastric lining. On the other hand they do contain foods rich in antioxidants, polyphenols, and other protective compounds that may support stomach function and prevent the breakdown of supportive stomach mucus.
Second, we invented blood thinners and painkillers. The widespread use of non-steroidal anti-inflammatory drugs (NSAIDs) like aspirin and ibuprofen, which inhibit prostaglandin synthesis and reduce mucus production and blood flow are known risk factors for stomach inflammation and ulcers. By way of contrast, the natural blood thinner nattokinase taken from the traditional Japanese breakfast superfood nato, improves blood flow and is not associated with stomach ulcers, and neither are natural anti-inflammatory painkillers like turmeric.
Modern lifestyles also involve much higher levels of chronic stress (from artificial light, EMFs, chemical toxins, social issues, etc) and certain compensatory habits like smoking and caffeine consumption, all of which can greatly exacerbate the risk of peptic ulcers via hormonal pathways.
Stress increases cortisol and adrenaline which inhibit vagal tone and delay gastric emptying which can prolong the time acidic contents remain in the stomach. Stress also decreases the production of prostaglandins required for producing protective mucus in the stomach. This happens via increased cortisol levels, elevated cytokine levels, and disruption of nitric oxide signaling. The elevated adrenaline induces vasoconstriction, which reduces blood flow to many internal organs including the stomach, impairing the delivery of oxygen and nutrients necessary for tissue repair and defense against acid.
Nicotine stimulates the production of gastric acid by increasing the release of acetylcholine from the vagus nerve, which in turn stimulates parietal cells in the stomach to secrete more acid. Nicotine reduces bicarbonate secretion in the duodenum, which is necessary to neutralize stomach acid as it enters the small intestine. It also causes vasoconstriction and reduces blood flow to the gastric lining.
Caffeine, especially from coffee and to a lesser extent black tea (green may be protective despite some caffeine due to high antioxidant levels, but would still avoid due to the caffeine which negatively impacts sleep), can trigger increased stomach acid and increased sympathetic stress responses via the production of adrenaline which as noted above leads to vasoconstriction and impaired blood delivery and thus impairment of the defense and repair of the stomach lining.
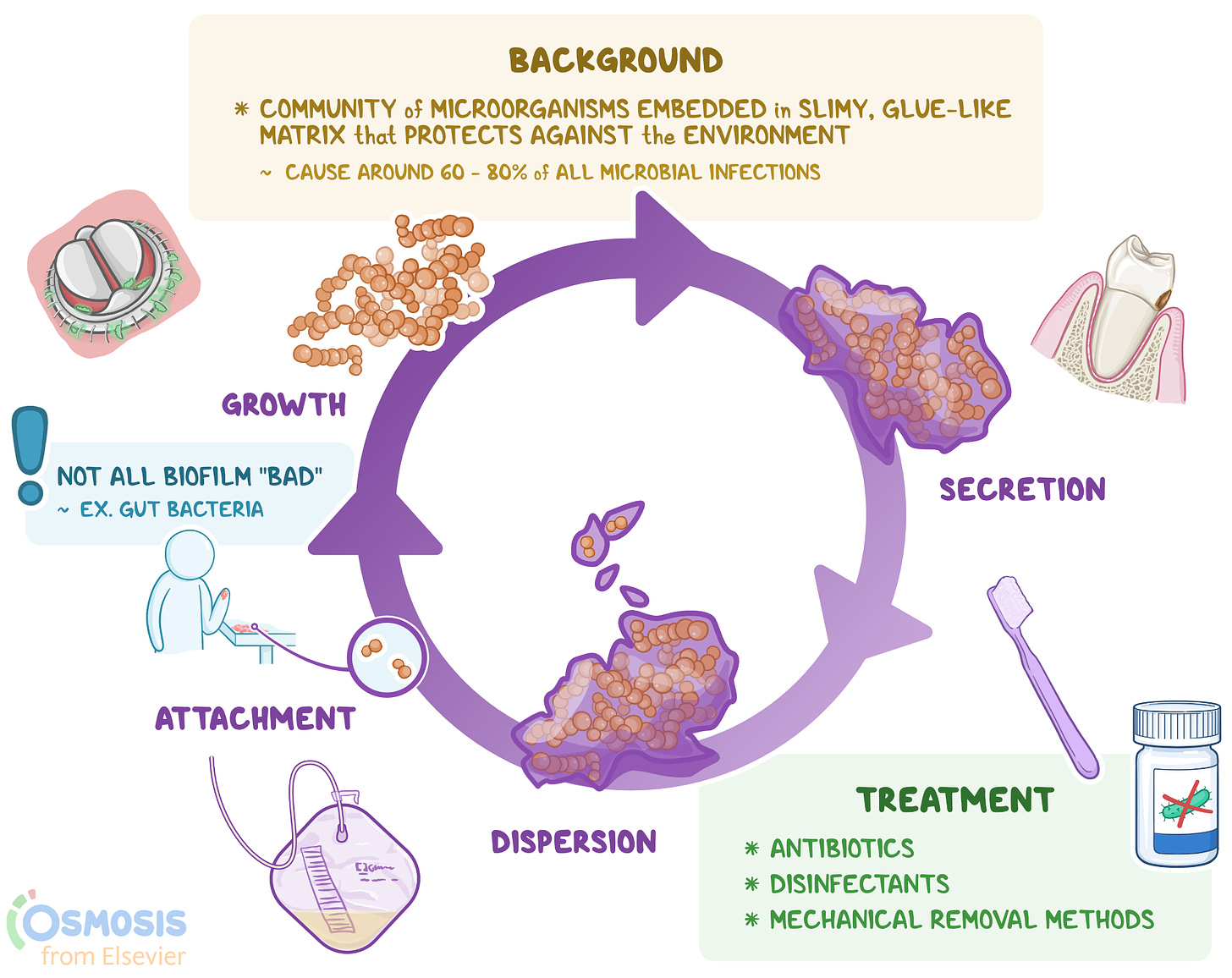
Another important factor may be that in traditional societies, the colonization of H. pylori might be maintained at a lower density, which could minimize its pathogenic effects while still allowing it to play a beneficial role in the digestive system. In contrast, modern factors like antibiotic use, which can kill off portions of the normal stomach and intestinal microbiota, might disrupt this balance potentially leading to higher levels of H. pyloricolonization due to the loss of competing microbes. This would be an analogous situation to killing off the wolves in Yellowstone leading to the increase in coyote, elk and deer. And we know how well that ended.
Finally eliminating H. pylori can have different consequences depending on the starting point.
In cases where H. pylori had caused “hypersecretion” of acid (as seen with duodenal ulcers), eradicating the bacteria can lead to a normalization or even an abnormal reduction in acid levels in the stomach, which could lead to problems digesting and absorbing nutrients later, particularly if acid levels fall further with aging. In other cases, where H. pylori had become much more overgrown and caused a disease called chronic atrophic gastritis, eradicating the bacteria might allow partial recovery of the acid-secreting cells, leading to a rise in stomach acidity.
Thank you for reading Dr. Syed Haider. This post is public so feel free to share it.
Treatments & Consequences
First of all it’s important to understand that there’s a systemic bias in modern medicine towards diagnosing something, nay anything, when a test is ordered. This is for insurance billing purposes and to justify the test - if a physician orders too many tests and they all come back negative the insurance companies may start sniffing around for insurance fraud.
In gastroenterology this manifests in literally every single upper endoscopy report I have ever seen showing the diagnosis of “gastritis”, or inflammation of the stomach, regardless what else was found or not. And always complete with pictures which may have included views of stomach lining that looked normal to the untrained or even trained eye, or may have demonstrated some vague reddening, perhaps from being poked with a probe for all I know.
But let’s say you actually have gastritis or peptic ulcer disease.
It should be exceedingly evident from the above treatment that there are numerous lifestyle factors involved in tipping the balance from normal to diseased.
Address those first. Don’t go killing your friendly neighborhood wolf.
Putting back what you take out isn’t always as easy as it was in Yellowstone. There may not be any readily available specimens to mix up into your own broth, and even if there are, there may not be any place in the ecosystem remaining for them to take hold. Other species will have filled the ecological niche and they guard their territory with zeal - often creating antibiotics to ward off invaders. This can be seen when taking probiotics that generally only remain resident in guts for a week or two.
Actually fully eradicating a resident microbe isn’t as easy as you might think though. In the case of H. pylori it requires a multi pronged attack for a prolonged period of at least a couple weeks with a combination of acid suppressing drugs and 2 or 3 antibiotics which wouldn’t usually be combined for other purposes. So it won’t usually happen by accident during treatment for some other issue.
Similarly the numerous rounds of (unnecessary) antibiotics most everyone has taken in their lives will definitely knock back their microbiomes, but won’t usually eradicate anything. Especially if someone has their supposedly unnecessary appendix, which is not just a vestigial revolutionary remnant, but serves as a microbial apocalypse seed bank to repopulate the gut, e.g. after severe bouts of diarrhea or in the modern context: antibiotic use.
Still the risk remains, and since almost every single outpatient infection (and even some inpatient ones) does not require antibiotics, it usually pays to be safe rather than sorry, and put that antibiotic in the trash can where it belongs.
If you risk it you may just knock off a keystone species somewhere in your body, like the Yellowstone wolves. Keystone species aren’t always at the top of the food chain, they may be seemingly unimportant members of an ecology, but they are like the social superconnectors in any human society: they know a lot of very important people. And those associates depend on them for their own survival. Knock out the keystone and an entire ecology can collapse just like an ancient Roman archway that stood for a thousands years without any cement will collapse if it’s central keystone is removed.
Recently I was introduced first hand to the wonderful world of natural medicine when I had a severe unremitting toothache that instantly resolved after crushing a clove of garlic with the affected tooth. Clove buds work too, and won’t make vampires or every normal person allergic to you as the powerful aroma seeps out of your pores for days.
There is the equivalent of this available for pretty much any infection, though in most it’s not needed. It’s better to put up with even a severe bout of the flu, bronchitis, gastroenteritis, pink eye, ear infection, sore throat, cellulitis or UTI, rather than stop them in their tracks. These bothersome symptoms are due to your own bodies immune system attacking, killing and expelling the invader that has taken up residence within you. Your immune system knows what it’s doing and your ultra-efficient clean up crews are always on hand to rebuild the tissue devastation they leave behind, typically within a day or two. If it does linger too long it usually means your immunity isn’t sufficient or the affected tissue has been too weakened over time to expell the invader and needs some help. In that case there are natural remedies for all of these that will wipe out any infection anywhere in the body. One example is colloidal silver, another is CDS, and there are many herbs as well. All dependent on proper dosing, frequency and duration.
What happens when you take the easy out too soon - an antibiotic or even an over-the-counter symptom suppressing medication for one of these run of the mill infections?
One, you may end up leaving the invaders where they are inside of you, i.e. you may think you’ve cleared up the problem because the symptoms recede, but the pathogen may be biding its time in hibernation, or simply multiplying in a hidden location where your immune system can’t find it, and such a situation will eventually lead to significant chronic tissue dysfunction - usually in the form of an “autoimmune disease”, which is really just the immune system finally waking up to the fact there are invaders on it’s home turf it needs to seek and destroy, i.e. it’s a chronci version of the acute issue created by inadequate and misguided treatments of many acute episodes.
Two: sure the antibiotic might actually kill them all off, but then you’re still left with the fact that you messed with Mother Nature’s patented and perfect intermittent detox and renewal plan.
It’s called survival of the fittest.
The fittest cells inside you survive and the oldest, sickest, most toxin and pathogen infested ones die off. It’s a form of autophagy, that hard won wonder therapy everyone raves about and fasts like maniacs to achieve. You get it for free when you’re sick, and it’s better and more thorough than almost all fasting-induced versions.
So next time you get sick, take the time off, rest, recover and go back to life cleansed and renewed.
And remember never kill the wolves. They’re man’s best friend, or at least they could be if you don’t provoke them.
Fractal Geometry
You’re not just one ecosystem.
Your body is a universe and you’re in charge. Organs are like entire galaxies full of planets and suns releasing biophotons within you that transmit information and energy just like our sun transmits information and energy to Earth and to us. Your cells again are like their own little universes, and their organelles like their own little galaxies. Wheels within wheels turning down to the quantum level.
Anything less than utter astonishment and reverent awe for such a beautiful and outrageously complex system will lead to misguided and harmful interventions. Such a system is irreducibly complex and should not be tinkered with in microscopic ways (pharmaceuticals and isolated plant compounds) from the macroscopic vantage point.
Instead use the macroscopic tools that are naturally at hand of lifestyle choices, inner work, and what’s present in the coevolved environment of our planet which will provide understandable information and instructions that your body can safely utilize.








No comments:
Post a Comment