"Blood Distribution of SARS-CoV-2 Lipid Nanoparticle mRNA Vaccine in Humans"
A summary of the newly uploaded preprint by Kent et al.
A new preprint hit the presses on July 27, 2024 entitled: “Blood Distribution of SARS-CoV-2 Lipid Nanoparticle mRNA Vaccine in Humans”.It was written by a group out of Australia and describes experiments that they did to show that the lipid nanoparticles used in the Moderna COVID-19 injectable products stick around and circulate on the blood. Shocker. They describe how so-called ‘anti-vector responses’ - such as the production of anti-PEG antibodies in the case of the modified mRNA lipid nanoparticle (LNP)-based injectable products - can be potent effectors in an immune response; be it beneficial, or not. As the authors point out, the long-term effects of boosting anti-PEG antibodies is not known.
What they did
They wanted to compare the decay rates of both the LNPs and anti-PEG antibodies to see whether the latter influenced the former decay-kinetics-wise, and how, if so. They took 19 people who got the Moderna bivalent ‘booster’ shot by intra-muscular IM-injection, and measured the modified mRNA by PCR and an ionizable lipid (LNP proxy) by mass spectrometry from plasma-derived samples. This small cohort of people all got at least 3 doses of monovalent COVID shots previously. The also took samples from everyone prior to ‘boosting’, and everyone was at least 139 days out from their last shot. This was their control.
One half-decent piece of news is that of the samples tested prior to the ‘booster’ shot being administered, none showed signs of modified mRNA according to their assays: a reverse transcription droplet digital PCR (ddPCR) method. The ddPCR step uses oil droplets to partition the reaction mixture, enabling the absolute quantification of target DNA without the need for standard curves and apparently is highly sensitive and accurate.
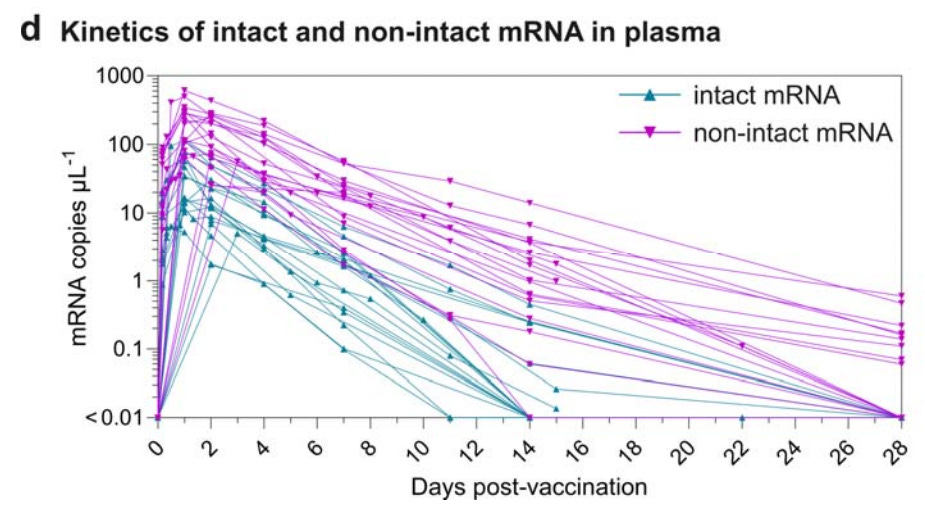
Four hours after the ‘booster’ however, modified mRNA was detected in all samples and in half of the people stuck around for 28 days.
To examine the LNP kinetics, they used a mass spectrometry-based lipidomics method to detect and quantify SM-102 lipids. For those of you who are new to this SM-102 ionizable cationic lipid, I have written extensively on this and you can read about that here and here and here and here.
This just means that they are measuring this fat in a biological sample using mass spectrometry and computational algorithms. Interestingly, they found an SM-102 signal as part of the pre-’booster’ background signal, which was much enhanced post ‘booster’ injection is all the subjects, peaked at what the authors call significant levels within 4 hours, and stuck there until day 4, and it wasn’t until day 7 that they returned to background levels.
They compared the kinetics of intact versus non-intact modified mRNA in the plasma and effectively mapped the degradation of intact mRNA to non-intact mRNA levels over time. I find it really interesting that the non-intact modified mRNA degrades less quickly. My mind went to frameshifting and N1-pseudoUs: maybe the swap-in made some weird-ass shaped mRNA all kinked out and made it more resistant to degradation?
They also used Enzyme-Linked Immunosorbent Assay (ELISA) assays to quantify anti-PEG antibodies pre- and post-’booster’. They are commonly used assays for detecting specific proteins in plasma. They found anti-PEG antibodies of the IgG type in 15/19 people, and 18/19 people of the IgM type, pre-’boost’. Once ‘boosted’, the anti-PEG antibody levels rose, and both IgG and IgM peaked starting from day 14 at day 28 due to injection spill-over into blood.
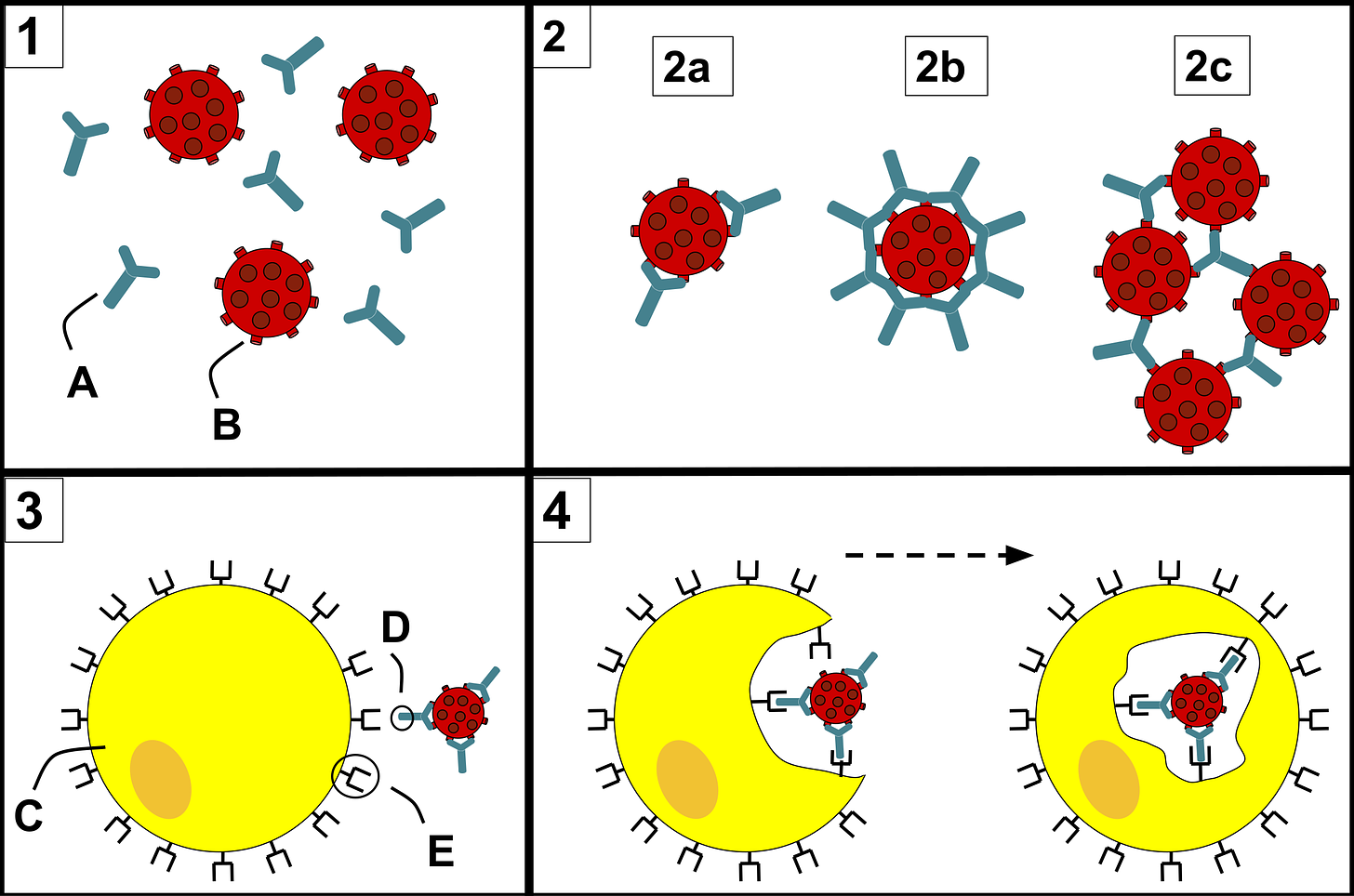
The authors had an idea that the anti-PEG antibodies would enhance the clearance of the modified mRNA LNPs via opsonization by phagocytes, but this was not really what they saw.
This suggests that the amounts of lipid nanoparticles distributed into blood were not high enough to have a major impact on the levels of anti-PEG antibodies.
Or maybe it was because the binding was suboptimal. Or maybe it was because the anti-PEG antibody levels were not high enough.
The modified mRNA lipid nanoparticles can be eaten by phagocytic cells once injected into the body via an anti-PEG opsonization mechanism inherent in these cells. Blood-borne product increases anti-PEG antibody levels so maybe the phagocytic capacity to take up LNPs affects LNP bioavailability itself to modulate the PEG immunogenicity.
They took the peripheral blood mononuclear cells (PBMCs) from all 19 people pre-’booster’ and checked them for ‘person-specific’ interactions. This is absolutely fascinating but I am not sure that I understand their meaning.
The lipid nanoparticles displayed a donor-dependent association with monocytes and B cells with minimal association with T cells, natural killer cells, and dendritic cells.
Does this mean that the anti-PEG antibodies, which are person-specific, create personalized LNP biocoronas that are associated with monocytes and B cells, or that the ‘person-specificity’ is more about the non-T cell involvement? The fact that they saw a negative correlation between anti-PEG antibodies and monocyte phagocytosis of the LNPs means that opsonization is not really playing a role, at least in the case of monocytes. It’s possible that the amount of LNPs circulating in the blood affect anti-PEG immunogenicity.
Some important take home messages
The similar kinetics of intact mRNA and the ionizable lipid in blood and the slow degradation of the mRNA suggests mRNA lipid nanoparticles remain intact and travel from injection sites or lymph nodes into blood stream within 4 hours post-vaccination.
The rapid dissemination of mRNA lipid nanoparticles in blood found in our study is consistent with the recent findings on the detection of mRNA in breast milk at 3–45 hours post-vaccination.
We detected low levels of mRNA in plasma 14-28 days after vaccination.
Taken together, our results suggest vaccine mRNA lipid nanoparticles recirculate for up to 1-month post-vaccination.
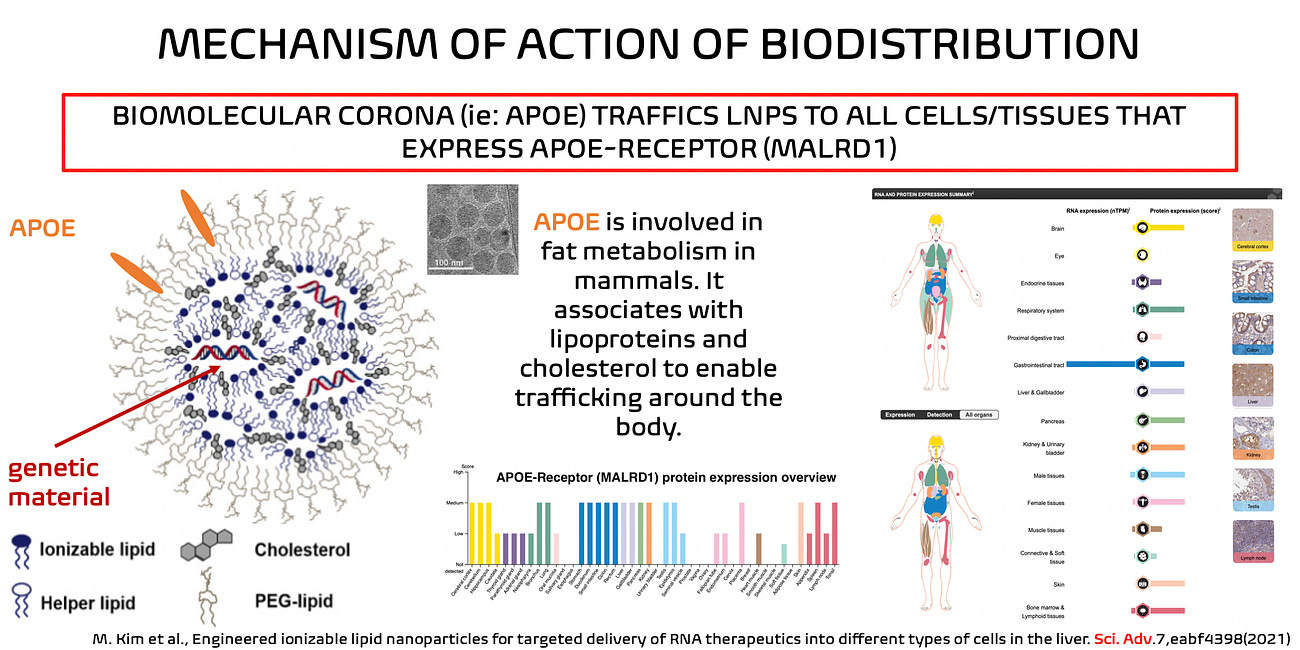
Ultimately, to me, this all has to do with the biomolecular coronas of the LNPs - both pre- and post-injection - into humans. They are very much like chylomicrons, and so there’s no reason to believe that they wouldn’t affect the immune milieu in a negative-balancing way, in my opinion, based purely on the fact that they aren’t meant to be circulating in our blood, and certainly not at any ‘high’ level. Please read this article.
All in all, this technology is new. Nothing of the pharmacokinetics of these LNPs were disclosed. The LNPs, the modified mRNA and the spike protein stick around.
Beware this platform - it is NOT plug’n’play - and tell your friends to beware as well.
Stephen J. Kent, Shiyao Li, Thakshila H. Amarasena, Arnold Reynaldi, Wen Shi Lee, Michael G. Leeming, David H. O’Connor, Julie Nguyen, Helen E. Kent, Frank Caruso, Jennifer A. Juno, Adam K. Wheatley, Miles P. Davenport, Yi Ju. Blood Distribution of SARS-CoV-2 Lipid Nanoparticle mRNA Vaccine in Humans. medRxiv 2024.07.25.24311039; doi: https://doi.org/10.1101/2024.07.25.24311039
Ju, Y.; Carreño, J. M.; Simon, V.; Dawson, K.; Krammer, F.; Kent, S. J., Impact of antiPEG antibodies induced by SARS-CoV-2 mRNA vaccines. Nat. Rev. Immunol. 2023, 23, 135
Long, S., Berkemeier, B. Development of a reverse transcription droplet digital PCR (RT-ddPCR) assay for sensitive detection of simian immunodeficiency virus (SIV). Virol J 18, 35 (2021). https://doi.org/10.1186/s12985-021-01503-5
Ju, Y.; Kelly, H. G.; Dagley, L. F.; Reynaldi, A.; Schlub, T. E.; Spall, S. K.; Bell, C. A.; Cui, J.; Mitchell, A. J.; Lin, Z.; Wheatley, A. K.; Thurecht, K. J.; Davenport, M. P.; Webb, A. I.; Caruso, F.; Kent, S. J., Person-Specific Biomolecular Coronas Modulate Nanoparticle Interactions with Immune Cells in Human Blood. ACS Nano 2020, 14, 15723

No comments:
Post a Comment